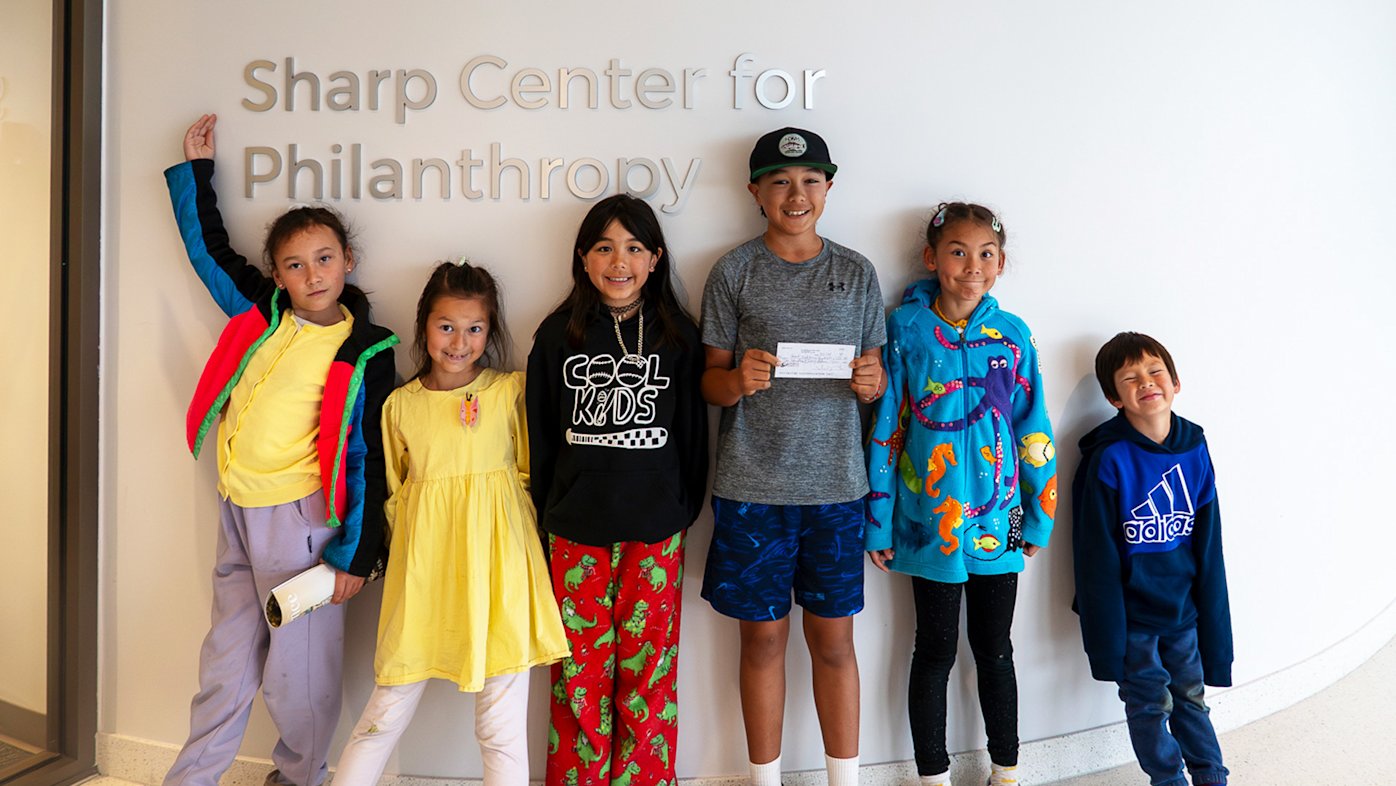
Lessons in philanthropy: Elementary students support Sharp
Six students at Barnard Mandarin Magnet Elementary School raised funds for oncology programs at Sharp.
Just saying the word colonoscopy makes some people feel uncomfortable. But consider this: Colorectal cancer is the second leading cause of cancer death in the world, yet it’s one of the most curable cancers if caught early through screening.
The gold standard for colorectal cancer screening is a colonoscopy. That’s because during the procedure, precancerous polyps can be removed if discovered, or cancer can be diagnosed if found.
However, most colonoscopy screenings don’t result in a cancer finding. If your doctor does find a suspicious lesion, such as a polyp, they remove it immediately during the colonoscopy before it turns into cancer. Your doctor can also take tissue samples for analysis to diagnose anything more serious.
Why do polyps need to be removed?
Most colorectal cancer starts from a polyp, a small clump of cells that forms on the lining of the colon. Oftentimes, they’re harmless; but over time, some grow and develop into cancer.
“A good quality colonoscopy is superior to other modalities in detecting not only cancer, but all different types, shapes and sizes of polyps, including small and large polyps, flat polyps and polyps that stick out,” says Dr. Michael Lajin, a board-certified gastroenterologist affiliated with Sharp Grossmont Hospital.
According to Dr. Lajin, there are three types of polyps:
Benign and not precancerous
Benign, but precancerous
Cancerous
“The precancerous polyps are called adenomas, and the larger the size of an adenoma, the more worrisome it is to contain cancer or turn into cancer soon,” he says.
How do I know if my polyp is cancerous?
During the colonoscopy, polyps are examined carefully to determine if they’re cancerous or noncancerous using advanced endoscopic imaging modalities, which are highly accurate. The procedure is minimally invasive and uses a small camera device called a colonoscope to examine the GI tract.
Dr. Lajin says if the lesion appears to be an invasive cancer, a biopsy is taken. Sometimes, the location is tattooed, so that a surgeon can easily find the location in case surgery is required.
If the diagnosis of cancer is confirmed, imaging with CT or MRI scans are performed to stage it. Staging a cancer determines how advanced it is and whether it has spread to other parts of the body. Following that, a team of experts, including an oncologist, a gastroenterologist and a surgeon, discuss the best treatment plan based on the stage.
In many instances, however, a polyp is usually found to be noncancerous, precancerous or possibly contain superficial cancer, also known as noninvasive cancer. In these instances, they are removed endoscopically during the colonoscopy and sent to a lab for a pathological exam, during which the polyps are studied for the presence of cancer.
What if cancer is discovered?
“If the pathology meets certain favorable criteria, the patient is cured endoscopically and can avoid having surgery — even if the lesion contains cancer — as long as the cancer is well-differentiated and superficial, and the resection margins are free,” says Dr. Lajin.
“In the past, patients with complex gastrointestinal polyps and early cancers were often referred for surgery,” says Dr. Lajin. “But because of exciting advances in endoscopic techniques, we’re now able to provide a less invasive alternative.”
For instance, Sharp HealthCare is among a small number of U.S. health systems that perform endoscopic submucosal dissection (ESD). ESD is a highly specialized, minimally invasive procedure that allows gastroenterologists to carefully remove the precancerous and cancerous areas in the gastrointestinal tract — sparing the organ and surrounding healthy tissue.
The new procedure has revolutionized treatment of complex polyps and early cancers in the upper and lower GI tract. A recent MD Anderson study also showed that more than 75% of patients with complex colon polyps could avoid surgery with ESD. Endoscopic Full-Thickness Resection (EFTR) is another minimally invasive endoscopic procedure performed at Sharp for difficult polyps that are scarred or polyps extending inside the appendiceal orifice or inside a diverticulum.
Who’s at risk for colon cancer?
Many people put off screening because they’re afraid of the results. But it’s important to keep in mind that detecting cancer early increases chances of survival and living a longer, healthier life.
The American Cancer Society says the risk of developing colorectal cancer is about 1 in 23 for men and 1 in 25 for women. Dr. Lajin adds that less than 1% of screening colonoscopies find cancer, and although adenomatous polyps are found in 25% to 30% of screening colonoscopies, less than 10% of them become cancer.
Colorectal cancer screening is recommended beginning at age 45. Talk with your doctor about your individual risk factors, such as a family history of the disease, to determine if you should be screened earlier.
Learn more about colorectal cancer; get the latest health and wellness news, trends and patient stories from Sharp Health News; and subscribe to our weekly newsletter by clicking the "Sign up" link below.
Our weekly email brings you the latest health tips, recipes and stories.